1. The first steps
During my internship at Hadassah, an accident occurred that critically influenced my entire professional future. Friday, January 18th 1957, on my way to the Department of Medicine, I slipped in the rain and fell. I felt instant pain in my left hip and could not get back on my feet. People on the street helped me, and I continued slowly on my way to the hospital, limping all the way. I started my routine work - drawing blood samples, preparing patients’ charts for rounds with the Professor, and similar chores. While doing all this, my limping became more obvious and arose general attention. Dr. Shlomo Rogel, at that time a medical resident and later professor and well-known cardiologist in Jerusalem, insisted that I get a radiogram. Finally, against my wishes, he sent me to the radiology department. The radiogram showed fracture of the femoral neck. I was not permitted to get up from the table. I was immediately transferred to the Emergency Room and was operated on that same day. Dr. Makin, chief of the orthopedic division, fixed my broken bone using a Smith-Petersen nail that remained in my body until the hip replacement in 2003. During the operation a number of complications occurred. As a result, I remained in the hospital for a whole month, and in a convalescent home for another month. For four months I was not permitted to use my left leg, and had to walk on crutches. The curriculum of my internship was modified, to enable me to be in “easier” departments during this difficult period.
Just at that time several resident positions became available in the Department of Surgery and a tender was announced. The candidates were interviewed in the Lecture Room of the Department of Surgery - the famous “shack” in the yard of the Ziv Building. Not doubting that my chances were excellent, I applied for the job. Judging from my student record and my performance as intern, there was no doubt in my mind that my residency position was assured.
When the judges’ decision was announced, the results amazed me. I was not accepted. The shock was beyond description. I felt that a great injustice had been done to me. I did not understand what had happened and could not accept the verdict. True, all the candidates were good, and the number of positions was limited, but still, the fact that of several available openings not one was offered to me, did not make sense. To me it seemed a terrible distortion of impartiality. For the next 29 years, long after recovering from the shock, the puzzle did not stop mystifying me. In 1986, when I had already been Chief of the Department of Surgery for 15 years, I happened to visit Professor Theodor Wiznitzer in Tel Aviv. We were drinking coffee and telling stories. In 1957, when the candidates for the position of resident were interviewed in Hadassah, Wiznitzer served there as a senior surgical resident. During the interviews, he entered the shack several times with some information for the senior surgeons and stayed for a while in the room. In this way he had an occasion to overhear some of the reasoning in favor and against the various candidates. When the candidate, Dov Weissberg, entered the room limping and supported by crutches, all the favorable impression from his good work as intern was forgotten in an instant. The judges saw only the limping intern supported by crutches, and nothing beyond. “Can this disabled young physician be a surgeon?” was their only thought. My fate was decided once and for all. From this moment on I had no chance to be accepted for a residency in Hadassah.
Had I been accepted in Hadassah, my career would probably have developed differently than in fact happened. Had I been... But whatever happened, had happened and it was irreversible. The senior surgeons remained my friends and through letters of recommendation and phone conversations helped me obtain a residency position. But not in Hadassah. This was the way that led me to the Rambam Hospital in Haifa, Department of Surgery “B”. Chief of the department, Dr. David Erlik (later Professor Erlik, founder of the Abba Khushi School of Medicine in Haifa) himself went through surgical training in Hadassah and all the senior surgeons there were his friends. Their recommendation was enough to ensure being accepted to his department. Indeed, this time there were no difficulties, and the tender was a simple formality. Because of my recent fracture, my military service was postponed for one year, and I could start the surgical residency immediately after my internship (Fig. 3).
One day in January 1958, just before the end of my internship, I went to Haifa for an interview with Dr. Erlik. He showed me the hospital and invited me to see some operations. The schedule for that day included a porta-caval shunt, a major and new operation. Dr. Erlik was the first surgeon in Israel to have performed this kind of operation successfully, and it was interesting to see him do it. I stood behind him and observed. One of the side-lamps obscured part of the operative field, so I shifted it slightly to the side. While I did this, the lamp hit the main headlight hanging from the ceiling, covered with a special opaque pane. The pane broke with great noise and shreds of glass fell in all directions. It was pure luck that no glass fell into the open belly. I wanted to bury myself on the spot. But Dr. Erlik tolerated the accident with patience and humor. Wasn’t this accident a sign from heaven, an omen forecasting the upcoming developments in Rambam?
* * *
I completed my internship in Hadassah on January 31st 1958 and on February 1th started the residency in Surgery. The Rambam Hospital had two Departments of Surgery: “A” and “B”. Department “A” took care of general surgery only. Department “B” (that of Dr. Erlik) handled, in addition to general surgery, also urology and vascular surgery. The background of this state of affairs should be explained, because it sheds light on Dr. Erlik’s distinctive personality.
In 1948, after the creation of the State of Israel, the British Hospital in Haifa became the Israeli Rambam Government Hospital. At that time the hospital did not yet have a separate urology service. Patients with urologic problems were treated, as in many other hospitals, in the Department of Surgery. To aid in the development of the hospital, a decision was made in the Ministry of Health, to open a separate urology service. Dr. Erlik from Hadassah became the chief of this new service. Due to his past experience in Hadassah, Erlik was equally proficient both in surgery and in urology, liked both, and had not the slightest intention of cutting himself off from either one of these branches. From the beginning, as the new chief, he admitted to his unit patients with both kinds of problems – general surgical and urologic. The new unit became not just a urology service, but a full-fledged Department of Surgery, with urology as part of it. In retrospect, the Ministry of Health recognized the fact that two Departments of Surgery are better for the Rambam Hospital than one and acceded to the new reality. But Dr. Erlik did not stop there. At that time a new branch of surgery started developing - vascular surgery - a novelty that appealed to Dr. Erlik very much. Within a short time this branch also became part of Dr. Erlik’s department, which by now had changed its name from Urology to Department of Surgery “B”. In later years, Erlik performed the first successful kidney transplantation in Israel. Accordingly, his residents had an opportunity to learn and gain experience not only in general surgery, but much beyond. And not just an opportunity; there was simply no other way. The program required more effort, but provided greater experience.
Surgery flowed in Dr. Erlik’s veins and his grasp of it was all-inclusive. He never hesitated to perform important, life-saving operations in any anatomic region outside of his domain. Chest surgery was not out of bounds, although he never studied it. I remember a soldier brought in as an emergency. He was wounded in the chest. Blood was flowing freely through the tube drain placed in his chest. The young man, with blood pressure near zero, was close to death. Without a moment’s hesitation Dr. Erlik opened his chest. The lung and pulmonary vessels were torn, and there was no way to stop the bleeding without resecting the lung. Erlik caught the pulmonary hilum (root of the lung) with his hand, pressed on it firmly and placed several heavy sutures on the entire mass of tissue, without trying to separate between the pulmonary artery, veins and bronchus. The bleeding stopped. He placed some more sutures to make sure that the bleeding would not restart. When the patient’s blood pressure began to rise, Erlik cut off the lung beyond the sutures and removed it from the chest. Then, in a voice expressing great satisfaction, he said: “This is the way to do a pneumonectomy”. To all present it was obvious that he had never before performed this kind of operation. He probably never even saw one being done. Indeed, this was not the way to do a pneumonectomy. But the bleeding did stop, and the soldier recovered and was discharged from the hospital. Many surgeons, among them chiefs of departments who had never learned how to do a pneumonectomy, would have stood there helpless, while the patient exsanguinated. But not Dr. Erlik. Erlik judged surgeons according to their performance in the operating room. He classified them either as “surgical stuff” or “non-surgical stuff”. If there ever was a physician made of “surgical stuff”, it was Erlik.
Dr. Erlik demanded absolute discipline and promptness. I remember the appendectomy of Dr. Fliegelman, chief of the Department of Psychiatry in our hospital. Dr. Erlik made the diagnosis while examining him outside of the hospital. The operation had to be done immediately. It was afternoon. Dr. Erlik was busy with some other business, which influenced his mood unfavorably. I was in the hospital on first call for emergencies. Dr. Erlik called me and demanded that the patient be on the operating table at 5 o’clock. Exactly at 5. I did all I could to complete the examination and bring the patient to the operating room on time, but an unexpected obstacle prevented me from achieving it: Dr. David Barzilai, a senior physician (later, chief of the Department of Medicine), decided to obtain an electrocardiogram before the operation. Due to some technical problem, it was impossible to make the EKG machine work and Barzilai, stubbornly refused to transfer Dr. Fliegelman from the Emergency Room to the operating suite without an EKG record. I told him that Dr. Erlik wishes to have the patient on the table at 5 o’clock, wants to start the operation exactly on time and is in bad mood. “Do you want the Chief of Department to undergo an operation without an EKG record?” asked Barzilai with derision. To my answer, “Yes, this is what Dr. Erlik ordered”, Barzilai did not even bother to answer. At 5 p.m. exactly Dr. Erlik entered the operating room, but the patient was not there: he was still waiting for the EKG in the Emergency Room. With shouts of rage Dr. Erlik ran to the Emergency Room and Dr. Fliegelman was immediately sent to the operating theater. Without an EKG. The operation started after 6 p.m. and throughout its entire course I felt Dr. Erlik’s anger.
* * *
When I came to the Rambam Hospital, all the work on the service, including emergencies on our days on call was done by three physicians: Dr. Singer - deputy chief of the department, Dr. Schramek - senior surgeon and Dr. Levin - second year resident, one year ahead of me. I was the fourth to join the team. Occasionally we had an intern for a month, but unlike Hadassah, most of the time there was no such luxury in Rambam. Just then Dr. Singer left for a sabbatical year in the United States, and all the work in the department of 45 beds, plus emergency calls, was carried on by the reduced team. To make the picture complete, it should be clarified that in those years, the Emergency Room of the Rothschild Hospital in Haifa was open for emergencies only one day a week, and the Carmel Hospital did not have an emergency room and did not accept emergencies at all. In 1958, the Emergency Room of Rambam Hospital was the busiest and carried the greatest burden of all the hospitals in Israel. There were, as I mentioned, two Departments of Surgery in the hospital, each with two residents. The nights on call were divided equally between the two departments. As senior surgeon, Dr. Schramek did not take emergency calls in the hospital (he was on second call at home). Each one of the four residents was, therefore, on emergency call every fourth night. When one of the residents was called to the Armed Forces for reserve duty (which accumulated to several months per year), we were on call every third night. No one thought that the Emergency Room should have a team of its own, or, at least one surgical resident just for itself. Nights on call were hard. The single surgical resident set into a perpetual motion was cruising between the Emergency Room, the operating room (emergency operations) and both surgical services, taking care of IVs and other urgent matters there. Today it is difficult to imagine the war-like situation that prevailed in the Rambam Hospital in those days. Many times, the work in the operating room went on uninterruptedly until morning hours, and through the windows one could see the rising sun, while no one attended to the Emergency Room, where patients were waiting...
I remember one early morning following a 24-hour period of uninterrupted work, I was assisting Dr. Schramek on a lengthy operation. In the midst of it, I fell asleep. I woke up from a roaring shout of Schramek in Yiddish: “Weissberg, shluf nisht (don’t sleep)!”. It was a rare occasion that a surgical resident actually slept while on a night duty; usually my bed remained untouched. On the day following the night duty, came the usual routine of morning rounds, drawing blood samples, operations, admitting new patients, and so on, until late afternoon or evening hours. In view of this intolerable situation, we went to Dr. Erlik to complain. We asked for a solution, which would make our work a little easier. His response was short and typical: “You don’t know how lucky you are, that you have something to do”. That was it. At the time we found it difficult to understand the great wisdom in Dr. Erlik’s words. Yes, I really mean it. Please, try to imagine for a moment people who have nothing to do. There are many. I know them and pity them much more than those young surgeons (including myself) who have no time to be bored. On our free evenings we found time for recreation, company, studies and hobbies. Indeed, I did have girlfriends, saw plays, read books and scientific journals, and more. Anyone who cannot bear this load, perhaps should not be a surgeon... Is this the way it should be? No, certainly not. But this is the way surgery was taught in the past; the way generations of surgeons have grown. And one can live with it. However, if good results are to be expected from such exertion and stress, two prerequisites must be fulfilled: friendly atmosphere and feeling of progress.
The senior surgeon in our department, Dr. Alfred Schramek worked hard and demanded a lot, not only from others, but from himself as well. He was broadly educated, had a fine sense of humor, spoke several languages fluently, loved music and understood literature and art. One could converse with him on any subject. In short, an intelligent person. But he was hard to work with, did not excel in politeness and in gentleness, and I, the most junior member of the team, felt it well. Dr. Dan Levin, although only one year ahead of me, let me feel his seniority at every opportunity. The atmosphere in our department and in the entire hospital was unpleasant and gave me the feeling of deprivation. Dr. Yaakov Singer, deputy chief of the department, was patient and friendly, but this did not help me when he was studying in America while I was trying to adapt to the uninviting environment. I recall many incidents that exemplify the Rambam atmosphere at that time. A patient with multiple injuries was hospitalized on our service. His broken leg was in a cast. Dr. Steiner, chief of the Department of Orthopedics was supposed to decide when to take the cast off. When the time came, Dr. Erlik ordered me to remind Dr. Steiner, which I did. Dr. Steiner gave me a scorning look and quietly said “good”. Then he waited patiently. On the day when Dr. Erlik made bedside rounds (“Grand Rounds” – twice a week), and when the entire retinue was in the 20-bed ward, a deafening noise of an electric saw burst suddenly in the room. It was Dr. Steiner, removing the cast. This was his way to demonstrate displeasure. Dr. Erlik stopped the rounds, approached Dr. Steiner and asked him what happened. To this Dr. Steiner answered: “Your junior resident gave me an order to take the cast off. That’s all”. Apparently the way I addressed him was not sufficiently polite, or, perhaps he preferred to be invited for a consultation, so that he would decide what to do, rather than being reminded what had to be done. But instead of pointing this out to me, he preferred to make this theatrical demonstration. Dr. Steiner had his own peculiar sense of humor, not always pleasant to his victims.
The Department of Orthopedics did not always have a resident on night call. Minor orthopedic emergencies were taken care of by the surgical resident, who called a senior orthopedist when needed. One evening I was called to see a patient whose leg was in a cast; his toes had become blue and swollen. The cast was apparently too tight and the foot was in danger. I opened the lower part of the cast with an electric saw, to relieve the pressure. I had seen this many times done by experienced orthopedists. The patient’s foot improved immediately. The next day, Dr. Steiner, short of staff, needed assistance on an operation, and I was sent to help him. After the operation he turned to me and said: “I would like to thank you for your help...”. Certain that Dr. Steiner was talking about my help in the operation that we had just completed, I answered: “Not at all, I will gladly help, whenever you need”. But Dr. Steiner kept talking: “... for your ‘wonderful’ help in opening the cast last night”, and continued criticizing my way of releasing the pressure, which apparently was not done in the best possible way.
With regard to the feeling of progress, the situation in Rambam surprised me greatly and gave me much to think about. Basic teaching methods, such as clinical sessions, bedside rounds with instruction, and preparation of subjects for seminars and lectures, in Hadassah were taken for granted. In Rambam of 1958 they simply did not exist. The active method of teaching introduced in Hadassah by Dr. Nathan Saltz, based on the North American residency training program, was initiated by William Halsted at the end of the nineteenth century. It put emphasis on active teaching and gradually increasing the responsibility of the surgeon-in-training (resident). There was an explanation for the lack of similar training program in Rambam: “You see how busy we are; there is simply no time for lectures and discussions. Treating patients comes before anything else”. This was certainly true: hospitals do exist first of all for the purpose of treating patients. However, even simple clinical or technical questions asked during an operation or at bedside rounds, were left unanswered, with a curt “I don’t have time now, let’s move on”. In short, I came to the Rambam Hospital to learn surgery, and after a short while, I had the feeling of marching in one place. One typical incident clearly illustrates the prevailing situation and the reasons for my frustration.
I had worked already for several months in the department and assisted in many inguinal hernia operations. On the day of the incident the operating schedule included, among others, two boys, 6-year-old twins, both with an inguinal hernia. Dr. Erlik was supposed to operate on both of them, and he chose me to assist him. While we were scrubbing for the first operation, I asked him whether I might operate on one of the boys. Dr. Erlik was visibly shocked by my question. His wet hands, one holding a scrubbing brush, stopped in midair. His eyes, greatly surprised, fixed on me while he asked: “Weissberg, are you crazy?! You want to operate on a hernia? A hernia is a serious operation! You have to learn first how to do it.”. If Dr. Erlik was shocked by my question, I was not less shocked by his answer. During my internship in Hadassah I had already operated on a hernia. It was customary that a hard-working, good intern who was interested in surgery, was rewarded toward the end of his rotation either with an appendectomy or a herniorrhaphy. Of course, this operation was done under the supervision of a senior surgeon, but it was the intern who performed the operation with his own hands, and thus learned. Due to the close supervision, the patient was not endangered in any way. The supervising surgeon (in my case Theodor Wiznitzer) was at the head. Had there been any difficulty, he would have taken over and completed the operation by himself. There were no such fancy games in Rambam.
* * *
Dr. Erlik had a number of principles with regard to surgical technique. One was the need for a sufficiently long incision at every operation. He insisted that a surgeon should have plenty of space available with a comfortable approach to all structures and a possibility to accomplish the purpose of the operation without compromising the patient’s safety. He pointed out jokingly that an incision heals from side to side, not from end to end. This principle is worth remembering now, in the days of minimally invasive surgery, when the tiniest possible incision is pursued above all other considerations. Without denying the advantages of minimally invasive surgery that did not exist in the 1950s, I often see surgeons, some with considerable experience and knowledge, who struggle helplessly with abdominal or thoracic organs because of their difficulty to reach some remote corner of the belly, sometimes causing great damage to tissues. All this, in order to avoid an incision of adequate length. The size of the scar seems more important.
Another of Dr. Erlik’s principles was related to the resection of the thyroid gland. A common complication of this operation is damage to the recurrent laryngeal nerve, the nerve that controls the muscles of the larynx. Injury to this nerve causes speech impairment and must be avoided. While operating on the thyroid gland, some surgeons separate this nerve to protect it against damage. Dr. Erlik claimed that looking for the nerve and dissecting it may be harmful; it is preferable to avoid injury by staying away from it. His results with thyroid operations were excellent, and I do not recall a single case of injury to the laryngeal nerve in our department. One day a well known surgeon from Boston visited Israel. Dr. Berlin was world-famous in the field of thyroid surgery. He insisted that it is essential to dissect the entire length of the recurrent laryngeal nerve, to see it clearly and thus protect it. Dr. Erlik invited Berlin to operate on one of our patients. Dr. Berlin demonstrated his technique clearly, and skillfully separated the nerve from the surrounding tissues. Everything seemed in best order. However, after the operation, the patient’s voice was hoarse, and a laryngoscopy 1 demonstrated paralysis of one of his vocal cords... This was the first time that I have seen both, how to separate and protect the recurrent laryngeal nerve, and this kind of complication. For many months we joked at the expense of the famous visitor. Apparently Dr. Erlik’s principle was worth more than the elegant demonstration of the nerve.
* * *
There was a general frustration among the residents. Our progress was far too slow, and we all felt immense starvation for operating. Itzhak Horowitz, a resident in the Department of Surgery “A” and later chief of surgery in the Rothschild Hospital, was two years ahead of me in training. Toward the end of his third year in surgery, he was still not permitted to do a cholecystectomy, and Itzik was “hot” to perform it. During one of his nights on call, a patient entered the Emergency Room. She complained of abdominal pain, vomited, and her abdomen was tender in the proximity of the gallbladder. The diagnosis of acute cholecystitis due to gallstones was clear. Horowitz had waited a long time for such a case, and his course of action was planned well ahead of time. He declared that the patient had acute appendicitis, wrote this diagnosis on the admission chart and, according to routine, took the patient to the operating room. Dr. Schramek was on second call at home, but Horowitz decided not to inform him about the case, at least for a while. He asked me to help him on an ”appendectomy”. At that time all abdominal operations in Dr. Erlik’s department were done through vertical incisions. Contrary to many surgeons, Dr. Erlik preferred this incision to all others. This fit exactly Horowitz’s plan. While realizing that the correct diagnosis was acute cholecystitis, he made the incision in the lower abdomen on the right side, as for an appendectomy. As soon as the belly was open, the appendix was found to be normal, as expected. Horowitz resected it, then said “let’s see what’s in the gallbladder”, and extended the incision upward. He found the gallbladder inflamed and full of stones, and started the resection. When this was nearly completed, he asked one of the nurses to call Dr. Schramek and to inform him that during a routine appendectomy an inflamed gallbladder was found and had to be resected. “Perhaps he wants to come, although it is not necessary. I can manage it by myself”. By the time Schramek arrived, the gallbladder was already out and the abdomen almost closed. Horowitz said: “Schramek, there is no need for you to scrub in, the gallbladder is already out”. Schramek was flabbergasted. He barely managed to utter the words: “Horowitz, what have you done?!”. “A cholecystectomy”, answered Horowitz, calm and relaxed. He did not show any signs of emotion. Eventually, this entire incident passed without further turbulence. I was too timid and too new in the trade for such tricks, but even much later, I have never reached this level of abusing the regulations.
During the first year of my surgical residency (not an internship anymore!) I was permitted to do appendectomies, but never a case of an inguinal hernia, hemorrhoids, varicose veins etc. Obviously, a cholecystectomy was beyond discussion. I worked in the Rambam Hospital, with an interruption, for a total of nearly two years. During the second year, likewise, I have not done any of these operations, that in the spectrum of general surgery are considered “minor”, except for three operations of inguinal hernia. These were awarded to me through the kindness of Dr. Singer who consented to help and instruct me. Appendectomies and three inguinal herniorrhaphies - this was the total surgical experience that I managed to accumulate during two years of such hard labor in the department of surgery. I felt I was walking in one place and wasting time.
I had enough of the Rambam Hospital and did not want to stay. But what could I do? I went to meet some of my former teachers, chiefs of several surgical services in Hadassah (general, thoracic and others). Conversations with them clarified to me ultimately that my way to Hadassah was blocked. If I was unhappy in Rambam, whose fault was it? Perhaps I was not good enough. And if I failed in Rambam, why should they risk it and take me on? But I believe that there was one other, major reason for their reluctance to specifically accept me as resident in Hadassah: it was their concern not to offend Dr. Erlik. There were plenty of other candidates whose acceptance would not offend anybody. Eventually I realized that my efforts in Hadassah were wasted; there was no point trying there. Should I start looking for a residency position in other hospitals in Israel? As a matter of fact I worried that a position in some other hospital might not necessarily be better than my present position in Rambam, but still, I tried. Several department chiefs in Tel Hashomer and in Beilinson answered my inquiries: “You have an excellent residency position in Rambam. Why are you looking for a job?”. Again, the same suspicions and the same reasons for not accepting me, as in Hadassah. There remained two options: to resign myself to the state of affairs in Rambam, or, to give up surgery and specialize in a different branch of medicine.
Or... there were before me physicians who went to specialize in the land of unlimited possibilities - the United States of America. The most striking example was Dr. Saltz from Hadassah. He did not really “go” to the United States, as he was born in New York, but he took his surgical residency there. I personally saw the truly impressive results of his training. I started inquiring among my friends who have spent various periods of study in North America, and I obtained a lot of valuable information and some good advice.
In order to work in the United States as a physician, a foreign medical graduate must first pass examinations both in medicine and in English, to satisfy the requirements of the American authorities - the ECFMG.
To expedite matters, I decided not to take the full advantage of my one-year postponement, but to leave the Rambam Hospital as soon as possible and get over with my military service. I contacted the military authorities and informed the Surgeon’s General Office that my disability is over. I feel well, I function well, and am ready to serve. Within days I was notified that the next Medical Officers’ Course is expected to open in October (a couple of months ahead), and received an order to return to service. I parted from my colleagues at Rambam with good feelings, we maintained contact and remained friends.
The Officers’ Course started on October 8th 1958. It was enjoyable and, unexpectedly, quite interesting. Part of it was military training, but a considerable portion was spent in the various departments of Tel Hashomer Hospital (later renamed Sheba Medical Center). From time to time I participated in operations and learned. For the first time I saw that clinical and surgical problems can be approached in different ways in various departments, and that these differences are discussed freely, rather than dogmatically dismissed. I learned to set broken bones and to immobilize fractures in a cast. I particularly enjoyed seeing lung operations elegantly executed by Dr. Yehuda Pauzner (Fig. 4).

Fig. 4. At the Officers’ Course; in the center Prof. Spira and the author holding a bottle of brandy.
After graduating from the course, I spent a short holiday in Eilat - my first visit there. Following that, I served in various units of the Air Force and took a course in Aviation Medicine. In parallel, I took emergency calls on weekends and nights in the Rambam Hospital, for a fee. In addition to the income, these calls helped me stay in touch with surgery and with the hospital.
In the beginning of 1960, due to some obligation on the part of the Israel Defense Force (IDF), the Medical Corps was supposed to provide a military physician who would work for one year in the Rambam Hospital as part of his military service. Dr. Erlik realized that after having spent eight months in his department, I had experience in taking emergency calls, could assist in operations, and could no doubt work more efficiently than some newcomer who had never worked in surgery before. Therefore, he requested from Col. Dr. Baruch Pade, the IDF Surgeon General, to send to Rambam not just any military physician, but me. Dr. Pade objected. According to the administrative routine in the Medical Corps, I was supposed to serve in a field unit and was not entitled to the “treat” of spending one year in a hospital, without committing myself to an additional period of service. But, when Erlik wanted something, he knew how to insist. No one could refuse him. To fulfill his wishes, I was sent to serve in Rambam for one whole year.
The first six months were to be spent on the neurosurgical service. This was new to me. During the years in the Medical School and in my internship I never spent any time on neurosurgery, and this was my first opportunity to learn something in this field. The sole resident who worked there, had just left in rage after a fight with the chief, and Dr. Eli Peyser remained alone. I came to fill the vacuum. Besides the chief, I was the only doctor on this 14-bed service, always full, all its patients seriously ill.
Dr. Peyser was a difficult person, short on patience, exploding easily. However, he was a very good surgeon and an excellent teacher. He taught me how to perform a thorough neurologic examination, management of trauma to the central nervous system, and more. He instructed me in reading articles relevant to our patients’ problems and invested great effort in my education. As his only resident, I participated in every single neurosurgical operation done in Rambam during the 6 months I spent on his service. However, as the only junior member of the team, I was on call every day and night, seven days a week. On days without operations, I could leave the hospital, but had to be within reach by phone, and not too far from the hospital. I found out to what ridiculous situations this can lead, when I was called from a theater in the middle of a movie. In the hospital they knew my seat number and called the theater. My girlfriend went home (she did not want to stay and watch the movie alone), while I went to the hospital for an emergency operation. A rather unpleasant experience.
For the remaining 6 months I returned to the Department of Surgery “B”. During my absence, Dr. Singer returned from the United States, and the general atmosphere became more tolerable. Also, the surgical team had expanded by a couple of new residents and I, as an old-timer among them, felt a certain superiority.
There were rumors that Dr. Singer may accept a position of a department chief in the Rothschild Hospital. During a coffee break, this possibility was a subject of conversation. When I uttered a few words, Dr. Yaakov Assa, a new resident, asked me with some derision: “Are you also interested in applying for the position?” I felt embarrassed, and did not know what to say. Instead of me, Dr. Erlik answered in Russian: “Nie tot soldat, kotoriy nie khochet byt’ generalom” (One is no soldier, if he does not desire to become a general). Suddenly, I felt like a victor, because even at that early time, there was a glimmer of hope in the depth of my heart to become one day chief of my own department. Erlik understood this.
While working in Rambam, I learned to keep Dr. Erlik in the highest esteem. Today I understand that he was one of the greatest surgeons I ever met. In my memory he remains engraved as a man of great wisdom and integrity, made of the most distinguished “surgical stuff”. He was a man of impeccable character, utterly devoted to his patients and always ready to support his pupils. All those who managed to endure his residency program, have reached important positions in surgery; many became professors and department chiefs. Also, one should remember that Dr. Erlik was the decisive factor in founding the Medical School in Haifa and its first dean. Without him, establishment of this important institution would have been delayed for many years. A great man (Fig. 5).
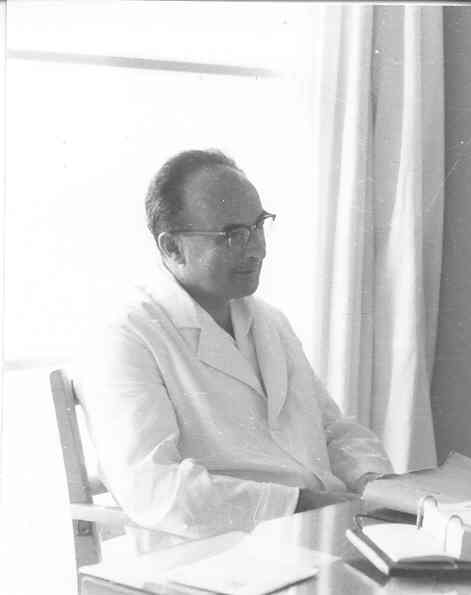
Fig. 5. Dr. David Erlik, 1960.
1 Observing inside of the larynx through a specially devised instrument.
