3. Training program with a curriculum
In the United States, the training program in surgery is determined by the American Board of Surgery. Chiefs of surgery in accredited hospitals are responsible for carrying out the requirements of the Board, while strict control is maintained over the quality of the training and the volume of operative experience of every resident. The minimum period of training is four years. However, every department chairman can extend it by a year or more, according to his own judgement and the needs of the hospital’s particular residency program. Toward the end of his training, the resident submits a detailed list of operations that he had performed by himself, and those in which he participated as the first assistant. A minimum number of each kind of operation is required and strictly adhered to. After approval by the Board, the resident is permitted to take the examinations that will qualify him as a specialist in his particular field 2.
Dr. David State, Chairman of the Department of Surgery at the Albert Einstein College of Medicine, had been trained by Owen Wangensteen at the University of Minnesota, was involved in scientific research and desired to transfer this tradition to his pupils. According to this concept, he added one year to the four required by the Board. During this extra year, every resident worked in surgical research (laboratory or clinical). The first two years of the residency were spent on rotation between the various surgical services and the resident gained clinical and operative experience. The third year was devoted to research, but the resident still spent nights on duty in the Emergency Room. This was to assure that he would not lose contact with clinical medicine. During the fourth year, as senior resident, he was again on the clinical services, and now his work included more advanced operations and greater clinical responsibility. During the fifth and last year, as chief resident, he had the ultimate responsibility for patients in his charge. He decided which operations to perform by himself, and which to let others do. The operating room schedule was checked and usually confirmed by the department chairman. In the most extensive operations, particularly those that he had not done before, one of the senior surgeons, qualified as a specialist, supervised and assisted him. The rule of chief resident was almost absolute. He divided the work between the other residents on the service, and devoted to their training as much or as little time as he desired, all according to his own judgment and sometimes caprice. He also evaluated the work and progress of the trainees under his control and reported this to the department chairman. These reports became part of the resident’s permanent record and influenced the chief’s decision - whose training to extend and whom to fire. In this connection I must mention Dr. Ronald Dee, the best chief resident I met during all the years of my training. He spent many hours introducing me to “practical” surgery and taught me many “secrets of the trade”, both in clinical approaches and in surgical techniques - this particular aspect of teaching that I had longed for at Rambam Hospital. We remain friends until this very day. There were also chief residents of a different kind, who took advantage of their position and coerced all kinds of personal services from their subordinates.
* * *
Three or four times a week, one hour was devoted to teaching and to the discussion of problems on the service; this included the mortality and morbidity conference, analysis of recently published journal articles (“Journal Club”), practical instruction in anatomy with dissection of cadavers, etc. We worked hard and did not have time to waste. As in the Rambam Hospital, this caused much fatigue. I remember a young Japanese intern, Dr. Takaro Suzuki, who was so tired that he fell asleep while examining a patient. I remember the strange view of an unconscious female patient stretched out on the examining table and lying on her, across the table, Dr. Suzuki, stethoscope clutched in hand, deeply asleep and snoring loudly. I tried to wake him up, pulled him firmly by the shoulder and yelled directly to his ear “Suzuki, wake up!”, but to no avail. The chief resident, Dr. Chinda Suwanraks, who heard me yelling, entered the room, evaluated the situation, and decided that whatever we do, Suzuki would not wake up. We picked him off the patient and gently put him on the floor. Then I, instead of my sleeping intern, examined the patient. This incident reminded me of that night in Rambam, when I fell asleep during an operation, but with one difference: Dr. Schramek had no difficulty waking me up. Suzuki, known for his drinking habits, was probably drunk at the time.
* * *
Whether a patient should be told the entire truth about his condition, is a matter of controversy. There are differences between the Israeli-European, and American approaches. What to tell a patient with an incurable disease? This is a humane-psychological matter, with deep roots in medical ethics. Considerable progress has been made in recent years, but the ideal solution has not yet been found. During the years spent in medical school and at the Rambam Hospital, I had been repeatedly told, how important it is to soothe patients and keep them calm. The truth should never be mercilessly thrown into the patient’s face. Hiding it was customary with a variety of diseases. If high blood pressure did not drop in response to treatment, the patient was not told so, for fear that this would cause the blood pressure to rise even more. This “soothing” approach reached various degrees. Among the physicians I met, there were great liars, small liars, and some, who tried to avoid lying as much as possible, but in general, the tendency was to make the patient calm at almost any cost. This was as important as the treatment itself, if not more so. The intention was always good. For what can be more important than protecting patients from the harsh reality of an incurable malignant disease? The thought behind this was that if the cruel truth becomes disclosed, the patient might commit suicide.
I remember a 50-year-old patient, admitted to the Rambam Hospital because of rectal bleeding. She had cancer of the rectum and was supposed to undergo abdomino-perineal resection of the rectum with creation of an artificial opening in the abdominal wall (colostomy) for bowel movements. This is unquestionably a major and traumatic operation. How does one obtain the patient’s consent for it, without disclosing to her the unpleasant diagnosis? The solution seemed relatively simple. The patient was told that she had hemorrhoids and needed an operation. Not a word that this will be an abdominal operation, nothing about its magnitude and about the artificial opening in the abdominal wall that will replace her anus forever. In those times there was no need for an informed consent; as a matter of fact, any signed consent was not considered essential and quite often was omitted. To the innocent suggestion of hemorrhoidectomy the patient consented without hesitation. How great was her surprise after the operation, upon discovering the long abdominal incision, the big open wound between the buttocks packed with gauze, multiple drains in the abdomen, nasogastric tube in her stomach, catheter in her bladder, two intravenous installations, and severe, unbearable pain. Desperate, she asked what happened. “Nothing. You had an operation”, answered one of the doctors. For whatever reason, this ”soothing“ response did not satisfy our patient. “So much suffering because of hemorrhoidectomy?” she asked. “Yes”. “Had I known what to expect, I would not have agreed to undergo this operation”, answered the patient. Such “impertinence” from a thickheaded woman who understands nothing in medicine! The doctor raised his voice: “Are you trying to teach us, how to operate on hemorrhoids?!” This response shocked not only the patient, but me as well. 3 While I did not know what answers to give to a patient who asked those reasonable and fully justified questions, it was obvious to me that the system of white lies and extreme arrogance exhibited by my colleague was a tragic error. It seemed clear that we should not tell the patient that she has cancer. But what should we tell her? How to prepare her for accepting the unbearable trauma, both psychological and physical? How to convince her to agree to undergo a necessary operation, if she does not understand its importance? I devoted much thought to these questions, but at that time did not find suitable answers.
A short time after starting my residency in New York, I came across a patient with cancer of the cecum. He was supposed to undergo resection of part of his large intestine (right hemicolectomy). When the time of operation came close, I approached him in order to obtain his consent - a written, informed consent, properly signed (this was the United States, not the Middle East!). I told the patient that we plan to resect the right half of his colon, gave him the properly filled consent sheet, and asked for his signature. “Operation? For me?” the patient laughed. “I do not agree”. “But you have intestinal bleeding and it might increase. We must resect the bleeding part of your bowel”. “Don’t worry”, answered the patient, “the bleeding has stopped”. “There is almost no doubt that it will recur. It will be more severe and endanger your life”. “Out of question! I will not have an operation”. The conversation lasted several minutes, during which I tried to explain how dangerous it is not to have treatment, while he, with growing impatience, responded that if I don’t stop bothering him, he would leave the hospital immediately, against medical advice. I went to a senior surgeon, Dr. Meyerowitz, and told him that Mr. V. refuses to sign consent for the operation. “Impossible”, answered Dr. Meyerowitz, as if he had never heard this before from a patient. We both went to Mr. V. “Dr. Weissberg tells me that you refuse to sign the consent for the operation”, said Dr. Meyerowitz. “Yes, indeed, I do not need one, my bleeding has ceased”. “But you have cancer of the large bowel and the bleeding will recur. Besides, the tumor will metastasise”. “Cancer?!”, answered the surprised patient and pointed his accusing finger toward me, “He did not tell me that I have cancer!” Following this, Mr. V. signed the consent form without further delay, and I felt like an idiot. Mr. V. did not become depressed. He did not commit suicide. His operation went smoothly and he lived for many more years, free of cancer. And I still enjoy this didactic lesson in surgical psychology.
Nowadays it is much more acceptable, even in Israel, to tell patients the truth about their condition, although not always the whole truth. There are still differences of opinion on this matter, but finally, the patients’ rights to participate in major decisions regarding their own health and life were recognized. It is their right to know the diagnosis and plans for treatment and to decide whether they wish to accept the treatment.
Psychology of the patient should be considered not only when dealing with consent for operation. I remember a patient with chronic illness who stayed in the hospital for a long time. One day, while she slept, a man came to visit her. The visitor preferred not to wake her up and left the ward. When the patient awoke, I told her that her son had visited her while she slept. “My son? I do not have a son”. “Well, the young fellow who comes to visit you every day, I thought he was your son”, was my innocent response. “Do I look so old?” asked the lady in a scared voice. “That is my husband”. I felt awful, and since then became more careful.
The hospital was always full of medical students, and the residents participated in their instruction (Fig. 10). I enjoyed this work and also learned from it myself. With time, my feeling that I learn best while teaching became stronger. It is relevant at all levels: teaching students and physicians, lecturing to nurses and instructing various other groups and individuals. When I assist a less experienced surgeon on an operation and teach him, I learn together with him. I always allowed my residents to operate from the beginning of their training. They never gave me reason to regret it.
* * *
Being in America gave me an opportunity to see world-famous surgeons operating. I took advantage of it from the earliest stages of my residency. From time to time I excused myself from work and went to see the “great” ones, usually recommended to me by friends who knew them. I spent one whole day in the Mount Sinai Hospital and saw the legendary “roaring lion” John Garlock perform several operations on the gastrointestinal tract. On another occasion I spent a day in the Beth Israel Hospital and saw Leon Ginzburg at work. In 1932, he, together with Crohn and Oppenheimer, described a new type of granulomatous inflammation of the intestine, known today as Crohn’s disease. Ginzburg expressed interest in the unexpected young visitor who came to see him operating. He asked several questions, invited me to assist him on one of his operations, and we drank coffee together. I may not have learned much from visiting these famous people, but the meetings enriched my memories.
* * *
Each year of my residency I was entitled to a two-week vacation. During the first year I decided to spend the holiday in Washington, D.C. and visit some of the historic sites, museums and other interesting places there. Three weeks prior to my planned trip, I bought a used car, Renault-Dauphin, in good condition. I was a new driver. I received my license about six months earlier, but had little opportunity to travel, and my driving experience was close to nothing. After several uneventful trips to Manhattan, I came to a hasty conclusion that I have mastered driving and can drive safely. My friends were surprised at my self-confidence and advised me not to get on the New Jersey Turnpike. But I had no doubts in my driving abilities. “After all, it is only a four-hour trip. What could possibly happen?” On the way to Washington, near Baltimore, I was stuck behind a truck, driving way too slow for my liking. I made a quick move to bypass it...
I woke up in the Emergency Room of the Hartford Memorial Hospital in Havre de Grace, a little town in Maryland. Because of a brain concussion, I did not remember the accident itself. I was lying on the treatment table and felt pain in my chin. The skin was lacerated and a doctor was stitching it up. We started talking. After a couple of sentences it became clear that we were both Israelis, and the conversation continued in Hebrew. The physician, Dr. Gunther (Gideon) Hirsch treated me as if I were his old friend. Instead of leaving me in the hospital for observation, as is customary after brain concussion, he took me to his home for “private” observation, where I stayed with his family for several days. On one of those days I went to visit the Johns Hopkins Hospital in nearby Baltimore. There, I had the opportunity to see Dr. Henry Bahnson operate on an aortic aneurysm. Bahnson was one of the first surgeons who performed operations on the aorta with success. I had heard about him earlier from a friend, an operating room nurse, who had worked with him a couple of years before and admired both his fine work and him as a person.
After recovery at Dr. Hirsch’s home, I still had a few days of vacation left. I went to Washington by train, because the remnants of my car could not be rescued. Dr. Hirsch remained in the United States and still lives in Havre de Grace where he served several terms as its mayor. We remain friends, and exchange holiday cards every year.
* * *
In January 1963 I spent my annual two-week vacation in Mexico. I visited archeological sites, places of religious importance, villages, markets, museums, the university campus and the new University Hospital in Mexico City. I saw examples of art and architecture like nothing I had seen before, and conversed a lot with people with whom I had no common language. The holiday was great, perhaps the most interesting and enjoyable in my whole life.
Touring the pyramids of San Juan Teotihuacan was particularly impressive. At noon I became hungry and entered the restaurant “La Gruta” located in a mountain cave. I looked at the menu. “Rabbit a la Gruta” attracted my eyes immediately. I recalled an event that occurred in 1950, when I worked in the zoology laboratory of the Hebrew University, together with Paul Yarden, a classmate and my roommate in the students’ dormitory. We studied anatomy of the mammals, and we were doing an anatomic dissection of a rabbit. I worked with diligence and followed the instructions scrupulously. My meticulous dissection arose Paul’s anger. “You are destroying the meat!”, he said. “Excuse me, I am following the instructions exactly, not destroying anything”. “Yes, of course, you are following the instructions and destroying the meat”, insisted Paul. It took some time before I understood that Paul intended to take the rabbit home to eat. One could understand this. In 1950 Israel was on a strict austerity regime. The immigration wave was at its peak, and in order to feed everybody, the government imposed rigid austerity measures with rationing of all food. The rationing of meat was particularly rigorous, with 100 grams (3.5 ounces) of meat per week, per person. Everybody was hungry for meat. Assuming that our rabbit was not poisoned, but had been killed by a blow on the head, and that prior to death it was a healthy creature (this we could not verify, but it was a convenient assumption), dissection completed, we took the dead animal home and cooked it. Neither of us knew how to cook a rabbit, and we did not add any spices. We just put the rabbit in a pot full of water and let it boil for several hours. We certainly managed to kill all the germs, but the food... A terrible stench filled our room and the entire dormitory floor, but this is the smell of rabbit, and nothing could be done about it. We tried to eat the “broth”, but its taste was so awful, that we poured it down the drain. But we could not afford to waste the meat. We managed to eat it, despite the bad taste.
And now... the menu! I wanted to taste a rabbit, a properly cooked rabbit, and nothing would stop my spirit of exploration. So this was my lunch for the day. The taste and the smell reminded me very much of that awful dinner in the students’ dormitory. I could not finish the dish. But the lunch added something to the spirit of my wonderful holiday.
* * *
My third year of residency (research laboratory) started in the summer of 1963. I desperately wanted to work in the vascular laboratory of Dr. Robert Goetz. In order to assure that I will be assigned to his laboratory (for there were several other, less attractive possibilities), I activated all my diplomatic abilities one year ahead of time.
First, I met Dr. Goetz, told him that I would like to work in his laboratory and asked him about subjects for research that might fit the 12 months allotted to me. Presented with several possibilities, I studied one of the subjects and prepared the project in general outlines. Dr. Goetz read my research plan, expressed reservations and criticized the weak points. This enabled me to introduce changes and to add some points. This went on several times, until the project was ready. At this point I went to Dr. State (Chairman of the Department) and told him that I was interested in spending my research year with Dr. Goetz, and that we were already well advanced in planning a research project on a subject related to blood vessels. My plot worked well. When the time came to allocate third year residents to the various laboratories, I was assigned to work with Dr. Goetz.
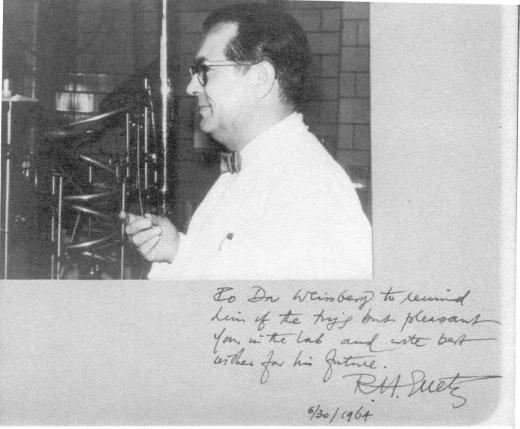
Robert Hans Goetz was born in Germany and studied medicine in Frankfurt. He completed his studies in 1933, the year the Nazis came into power. He was not Jewish, but because of his democratic-liberal ideas and his opposition to the Nazi regime, he left Germany in 1934 and worked for several years in research in Switzerland and in England. In 1938 he moved to South Africa, where for the next 20 years he directed the cardiovascular research laboratory at the University of Cape Town. The results of his work became famous among scientists and he won international renown. In 1958 Dr. Goetz moved to the United States and assumed a position at the Albert Einstein College of Medicine in New York, where he became chief of the surgical research laboratory and of the vascular surgical unit. A brilliant man abounding in original ideas and a charming person. (Fig. 11).
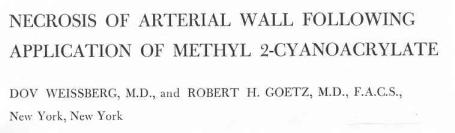
In surgery, those were the times of excitement with the use of glue in place of sutures for joining tissues. Dr. Goetz’s dream was to create a safe vascular anastomosis 4 in coronary bypass operations. 5 The bypass operation was considered difficult, and Goetz believed that if a sutureless technique could become feasible, it would make the operation easier. Our purpose was, therefore, to create a coronary anastomosis, using surgical glue instead of sutures. The experiments were carried out on dogs, under general anesthesia. Besides me, two other residents worked in the laboratory: Ruben Hoppenstein, a resident in neurosurgery and Mo (Mohammed) Amirana, a Pakistani, resident in thoracic surgery. Each one helped the two others in their experiments, and we published some of our articles together. My project on vascular anastomoses begun with a failure: the dogs survived the operation, but were dead within several days. At autopsies we found that the anastomoses disrupted because of necrosis of the tissue that came in contact with the glue. The adhesive, methyl-2-cyanoacrylate, in short “preparation E-910” was no good. The project was, therefore, changed: from then on, I studied the adhesive itself, and its effect on tissues. I found that application of E-910 to blood vessels and other tissues caused abscesses and necrosis. There was no point in using it. Because the “revolutionary” glue was in widespread use in many laboratories in the United States, we described the various aspects of our findings, presented them at three international conventions and published six articles in surgical journals (Fig. 12).
In spite of the heavy work load in the laboratory, the emergency night calls and the usual teaching sessions in the hospital, I felt considerable relaxation throughout the entire year. The working hours (morning till afternoon) were convenient, and the work was not nearly as strenuous as that on the wards. There was enough time for socializing, seeing plays and excursions - particularly on weekends. I tried my abilities at skiing, with fracture of my leg as a result (Fig. 13).
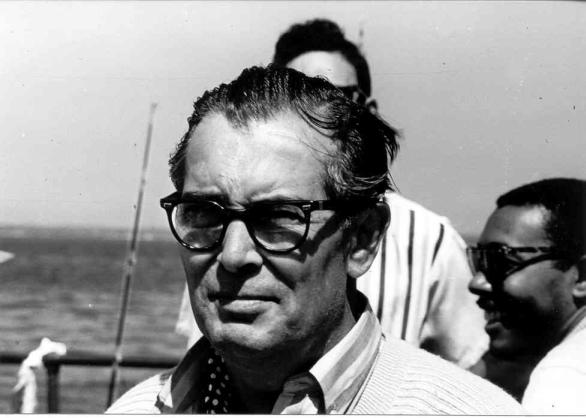
The work in Dr. Goetz’s laboratory was an ongoing pleasure. He was a great teacher, and I had a very rewarding year. Toward the end of the year he took the entire laboratory team for a day of fishing (Fig. 14).
My friendship with Dr. Goetz lasted a lifetime. I visited him shortly before his death and found him active, of clear mind and, as always, young in spirit. He died in December 2000, at the age of 90.
* * *
During the fourth year, as senior resident, I no longer had to do the boring, routine work. On the other hand, I operated more, my operations were more extensive, and I also taught more. This greater responsibility had serious implications regarding matters of my judgement.
I was on a rotation in the Lincoln Hospital in southern Bronx - a neighborhood of poverty, crime and violence. This was an important and useful rotation because of the wide exposure to cases of trauma, that were rarely encountered in the more civilized and quieter neighborhood of the Albert Einstein. I remember a black boy, 16-years-old, shot in the abdomen. I operated on him late at night. Abdominal exploration disclosed extensive laceration of the blood vessels supplying the left kidney, with profuse bleeding. The kidney itself was not damaged, but repairing and connecting the blood vessels was out of the question. The patient was close to death. I had to resect his kidney, which was a life-saving procedure. The bleeding stopped, and the boy recovered. At the weekly mortality and morbidity conference, one of the senior surgeons, Dr. Donald Perlman pointed out that I had resected a “healthy” kidney of a 16-year-old boy. To my explanation that otherwise the bleeding could not have been controlled and the boy would have died, Dr. Perlman shouted in anger: “But you did stop the bleeding! How did you accomplish it?” “I put a clamp on the blood vessels proximal to the laceration site.” “And why did you not use the DeBakey clamp?” This is a special clamp for blood vessels that enables a gentle grasp to stop bleeding, without crushing the vessel. Then one can repair the torn vessel by sutures. In our case this solution was not possible, because the vessels were totally destroyed. There were no sufficient stumps to put sutures in. Had I tried to repair the vessels, the bleeding would have restarted, and the boy would have died. But Dr. Perlman’s outburst gave me something to think about. I learned something. Two years later, while serving a thoracic residency at the University of Mississippi, I operated on a patient shot in the left lung. Upon opening his chest, I saw that the bullet had passed through the pulmonary artery 6, which was bleeding profusely. Rather than resecting the lung, I put the DeBakey clamp on the bleeding vessel, as suggested by Dr. Perlman at the Lincoln Hospital. The bleeding stopped. I sutured the torn vessel gently and removed the clamp. The lung was saved and the patient recovered. While a similar approach was not feasible in the boy who lost his kidney, Donald Perlman’s screaming planted a seed of an idea in my head.
Anticipation of a major operation that I had not performed before, may end in a great disappointment, if the operation is cancelled. I remember a patient with cancer of the rectum, on whom I was supposed to perform my first abdomino-perineal resection. I prepared myself well by reading the relevant articles and book chapters. The morning of the operation, I approached the patient for a little chat. He complained of chest pain and shortness of breath. Appropriate tests were performed immediately and disclosed myocardial infarction. The operation was cancelled, and the patient received treatment for his heart attack. Despite all efforts, he died on that same day. I was disappointed to lose this major operation, supposed to be my first of this kind. The senior surgeon in charge of the patient told me “Do you know how lucky you are that the patient died before you operated on him, rather than during, or immediately following your procedure? Imagine what everybody would have thought about you and how it would have effected your further progress”. Small consolation...
Good working relations and cooperation are of utmost importance and influence the conduct of an operation and its results. Among the many surgeons at the Albert Einstein there was one, with whom I did not manage to establish good relations. Dr. R. did not miss an opportunity to make my life difficult. He always managed to find flaws in my work and criticized every aspect of it, both in the course of operations and on the wards. I never found out his reasons for this strange conduct, so different from all the other senior staff members. Naturally, I did not like to work with him and tried to limit as much as possible my contact with him, but this was never easy, and not always possible. My efforts to avoid Dr. R. became particularly important in the case of Mrs. Angelina Occuizzo, a 72-years-old Italian woman who had cancer of the lower end of the esophagus, where it connects to the stomach. An adequate operation for this tumor involves resection of the lower half of the esophagus and two-thirds of the stomach, with translocation of the remnant of the stomach into the chest and its connection by anastomosis to the remaining part of the esophagus. This is a major operation and a challenge for every surgeon, particularly a young one who had not completed his residency yet. Dr. R. was in charge of this patient, and he was supposed to help me with her operation. I had no earlier experience with this kind of operation, and I particularly worried that if Dr. R. will start his “games” with me, the operation might end in a failure, perhaps even result in the patient’s death. For the benefit of the case it was important to get him out of the way and prevent his participation in the operation. For this particular operation I desired the help of Dr. Louis DelGuercio, whom I respected very much as a knowledgeable and experienced surgeon, and as an excellent instructor. My relations with DelGuercio were good, and at operations we always got along very well. But how to neutralize Dr. R.? How does one prevent a senior surgeon who is in charge of a patient, from participating in this attractive and challenging operation? There was no doubt in my mind that Dr. R. would not renounce his right voluntarily. In order to avoid him, I had to use a stratagem.
I decided to act as a naive “boy” and pretend that I was not aware of Dr. R.’s role in the case. While ignoring him, I went to Dr. DelGuercio, told him about the patient and asked when can we operate on her. DelGuercio was not stupid. He knew very well, who was in charge of the case, but decided to cooperate. He chose a day convenient for the operation and gave me detailed instructions on how to prepare the patient. Our cooperation brought good results. The operation was uneventful, without difficulties or surprises. I enjoyed and learned. The postoperative course, likewise, was smooth.
Dr. R. boiled with anger. Dr. State, Chairman of the Department, was on a sabbatical year in Los Angeles, and Dr. R. complained to the acting chairman, Dr. William Metcalf. I had committed a serious transgression, a sophisticated trick, connived in collusion with DelGuercio. Dr Metcalf was an austere man, rarely seen with a smile, and all residents were afraid of him. But he was unbiased. He usually appreciated my work, and always treated me with fairness. Still, I was quite scared when he called me to his office, less than 24 hours after the operation. Luckily, I was not the only offender. Dr. DelGuercio, the senior surgeon on the case, cooperated with me. Dr. Metcalf did not investigate my transgression in depth; he just wanted to know why I asked Dr. DelGuercio, not Dr. R., to assist me. I took advantage of the situation and told him about Dr. R.’s unfairness toward me and about our unhappy working relations - the plain truth. I did not have any remorse about “telling” on Dr. R. After all, I wasn’t the one to initiate the conversation with Dr. Metcalf. He had invited me and I only answered his questions. We conversed in good spirits and I wasn’t even reprimanded. However, Dr. Metcalf made it clear that only the surgeon in charge of patient, and no other, should be called upon to assist the resident with the operation. He also stressed that in the future I must behave in accordance with the department rules and not make changes on my own initiative. When I told DelGuercio about the judgement, he laughed. And Dr. R. learned that he should not give me unjustified trouble. Our working relations improved instantly. From then on, when we operated together, he behaved decently. Dr. Metcalf probably pointed out to him his past unfairness toward me.
Angelina Occuizzo was discharged from the hospital after an uneventful recovery and remained a grateful patient. This woman who had never learned to read and write, sent me every year a Christmas-New Year’s card written by her daughter. The daughter added relevant information about her mother’s progress and so enabled me to maintain a follow up. Angelina lived for another 20 years. She died at the age of 92, free of cancer. Her daughter and I continue to exchange Christmas and New Year cards now for more than 35 years. So perhaps it is justified to use a “non-kosher” trick from time to time...?
* * *
An essential part of a surgical residency is cooperation between a senior surgeon and a resident, in which the resident is obliged to obey. This is part of learning. But on occasion it can lead to mishaps with serious consequences. I operated on a patient with a mass in the cecum (part of the large bowel). The mass was demonstrated on the barium enema study, and the patient was scheduled for a right hemicolectomy. The senior surgeon who assisted me on this operation had worked earlier in a most prestigious oncologic hospital in the New York City and had extensive experience in oncologic surgery. He was aggressive in all that concerned cancer and usually favored radical, extensive resections. During the operation, I wanted to be sure that the mass is, indeed, cancerous, and suggested that we send a small section for an immediate microscopic examination, while we continue to operate. My instructor looked at me with surprise, smiled and asked: “Are you in doubt? What else can it be?” “It could be a periappendicular abscess, a complication of appendicitis in the past.” “Really?” He took the mass in hand, moved it from side to side and asked: “How many times have you seen an abscess that can be grasped by hand and moved from side to side?” “Never”, I answered. “So, what is this mass?” “This is cancer of the cecum.” “And what is the treatment of cancer of the cecum?” “Right hemicolectomy.” “Very well then, do it.” So I did. The postoperative course was uneventful. After several days we received the report of histologic examination: the resected mass was not cancer, but an abscess, the result of perforated appendicitis...
The same bold and aggressive senior surgeon was embroiled with another case, similar, but with more grave implications. This time, fortunately, I was not involved. The “honor” was bestowed upon another resident. The patient was admitted because of rectal bleeding. Examination disclosed an ulcerated nodule in the rectum. The finding was strongly suggestive of cancer. The appropriate treatment for cancer was abdomino-perineal resection of the rectum with creation of colostomy for bowel movements. The resident who examined the patient suggested biopsy of the nodule in order to confirm the diagnosis, but the senior surgeon was amused: “What else can it be? It is a clear-cut case of cancer.” The operation was technically a “success”, but histologic examination disclosed an inflammatory lesion in the rectum, with no evidence of cancer. The patient recovered uneventfully, but remained without the anus and with a permanent colostomy...
* * *
The ultimate responsibility for all the patients on the service rests with the chief resident. This brings certain rigidity and inconvenience to the routine of his work: he has no nights off. The chief resident is on call at all times, day and night.
There were three surgical services in the Department of Surgery at the Albert Einstein College of Medicine, with a chief resident on each service. Every night one of the three remained on active duty in the hospital. The other two left hospital at the end of the day, but remained in contact by telephone with their respective services. While during the earlier years I had enough time to see plays and occasionally a movie, this became impossible during my final year as chief resident. However, I did not grasp this new reality from the beginning. I learned it from experience.
On Broadway they were showing the musical “Oklahoma!”. I bought two tickets and invited a nice medical student who was on a rotation on my service. I had great hopes for an interesting and pleasant evening. Toward the end of the day I made bedside rounds and discovered a complication in one of my patients: bleeding after a stomach operation. I had to operate on him again, immediately, to stop the bleeding. My hopes for the pleasant evening evaporated in a moment. I apologized to the student (this was the end of our friendship), gave the theater tickets to a junior resident who was free that evening, and stayed in the hospital to operate. The next morning the young physician told me that he and his wife had enjoyed the show immensely...
The bleeding that prevented me from seeing the show had three consequences. First, I never saw the musical “Oklahoma!”. Too bad. Second, for the rest of the year as chief resident I never bought tickets for another play. For the whole year I did not see a theater performance. Never mind, one can live without it. But the most important result of that bleeding was the third one: three years later, when I met Milka, I was still a bachelor. Pure gain. Since then I believe in luck.
* * *
Lung operations caught my interest long before the beginning of my surgical residency. As early as my internship in Hadassah, chest surgery appealed to me. The thought remained hidden in some corner of my brain and started developing while I made my first steps in surgery. The idea matured during my annual rotations on the thoracic surgery service at the Albert Einstein. During the year in the research laboratory it was already clearly established in my mind. I decided to specialize in thoracic surgery. I immediately started searching for an attractive residency position. At this time I met my old friend from Hadassah, Yona Fruman. She used to be an operating room nurse, but at that time worked as a flight attendant in El Al and visited New York frequently. In the spring of 1964 she told me that Dr. Morris Levy from Tel Hashomer has been appointed as chief of the Department of Thoracic Surgery in the Beilinson Hospital in Petah Tikvah. He was expected to return shortly to Israel from the University of Minnesota. I remembered Dr. Morris Levy well from the time I spent in the department of Dr. Pauzner in Tel Hashomer, and had seen him operating on a number of occasions. In 1960 he left Tel Hashomer to work at the University of Minnesota Medical Center in Minneapolis. The news about his imminent return to Israel electrified me. The moment I heard it, I decided to go to Minneapolis to meet Levy and discuss with him the possibility of working with him in the future. Yona suggested that I hurry, because Levy was planning to return to Israel within the next couple of weeks.
Several days later I was on the plane to Minneapolis. Levy remembered me from Tel Hashomer and met me in a good, agreeable mood. Toward his return as department chief, he would need a new team of surgeons. He suggested that I stop my surgical residency, return with him to Israel and join his staff. “Why waste your time here? Come to my department and you will learn something”. His offer was kind and friendly, but I had different plans. Ahead of me were the best two years of my residency: senior and chief. To discontinue at this point, after I invested so much time and effort and became well settled at Albert Einstein – did not make sense. Also, I was planning to continue my surgical education – residency in thoracic surgery – in the United States. My purpose of meeting Dr. Levy was to establish contact toward a more remote future, rather than an immediate, drastic change that would involve interruption of my residency. Thus our meeting did not end in a matrimonial union. But we decided to maintain contact, with eyes on the future.
After the meeting, Dr. Levy showed me the research laboratories of the University of Minnesota. From there I took a short trip to Rochester, to see the Mayo Clinic. I spent a whole day there and became immensely impressed by this legendary institution. I believe that every physician in the world should strive to visit it at least once in a lifetime, to see and learn from its rich history and wonderful organization. Medicine at its best.
2 Male gender was used in this paragraph, as nearly all surgeons and trainees in surgery (well over 90%) were men. In the 1960s a female surgeon was a rare exception.
3 I wish to emphasize that this shocking story is not invented. It really happened, exactly as described.
4 Vascular anastomosis: connection of blood vessels, allowing blood to flow between them.
5 Recently an interesting article was published about Dr. Goetz and his scientific work: Igor E. Konstantinov: Robert H. Goetz: The surgeon who performed the first successful clinical coronary artery bypass operation. Ann. Thorac. Surg. 2000; 69: 1966-1972.
6 The main artery supplying blood to the lung.